3 min read

A decade after its creation, it’s time to take stock of the Center for Medicare and Medicaid Innovation’s (CMMI) progress and challenges.
That’s exactly what leading researchers and healthcare industry experts did in a recent report from the Leonard Davis Institute (LDI) at the University of Pennsylvania. Coming on the heels of another recent report shepherded by Leavitt Partners that charts a course for episodes of care payment programs in Medicare, there now seems to be broad consensus from policy makers, healthcare experts and practitioners on alternative payment models (APMs) that Medicare and other public and private sector payers and purchasers should focus on as we chart the course for the next decade.
Pillars of payment reform
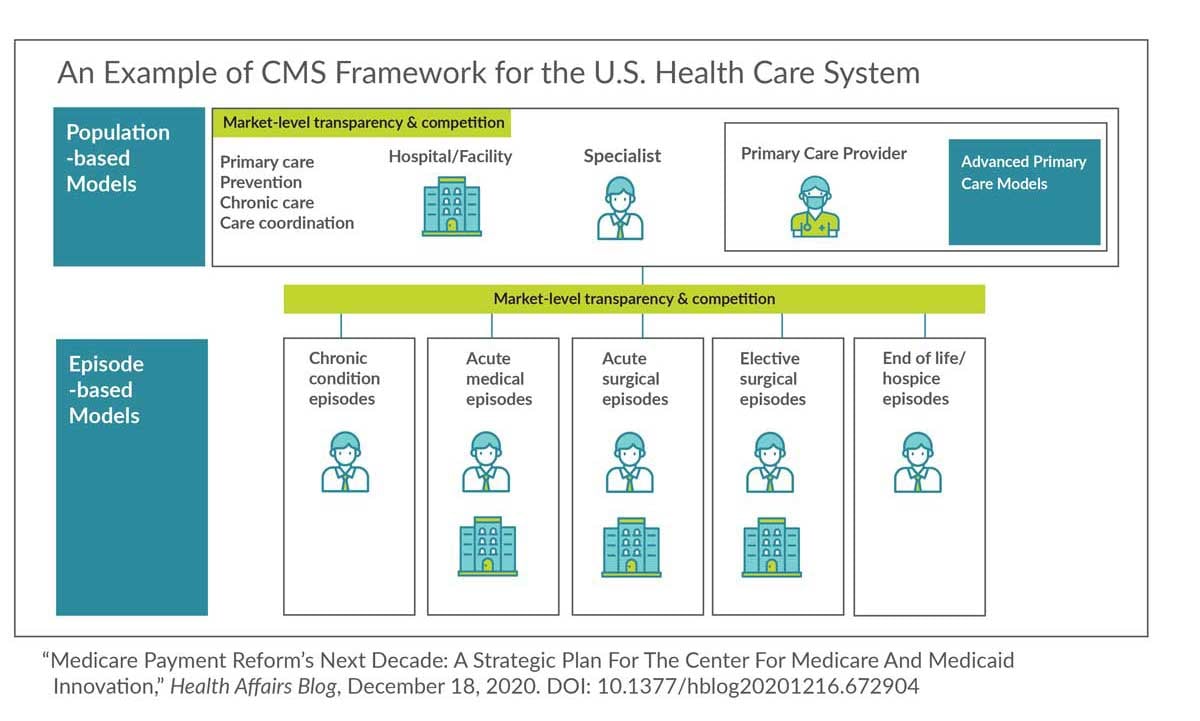
Employers should not be surprised by the findings, as they reinforce what they have been working to implement this past decade and what they have expressed as priorities for the next decade: Namely that a better path forward is built upon key pillars of payment reform - advanced primary care and episode/bundled payments for specialty care, both as part of an overarching total costs of care model.
These analyses cut through the chaff of APMs, making sense of the last decade of experimentation and offering an experienced-based path forward. As those toiling in this field can attest, this is not easy work. Sometimes, in the enthusiasm of sowing a thousand seeds, we forget that the overabundance of a crop is as much of a problem as no crop at all. That’s especially true when the seeds from different crops become entangled - an analogy applicable to what has happened with the proliferating and unmanageable set of alternative payment models supervised by CMMI.
The private sector has been more methodical and restrained, in part because the third-party payers they rely on are ill-equipped to manage even the most basic APMs. To an extent, the private sector has suffered from a very meagre crop and it’s time to sow more seeds and dig deeper.
A call for unification
The recent LDI report recommends discipline in the portfolio of APMs, and that the federal government use the full force of its purchasing power through all of the health plans it manages (or where it exerts some control). That includes Medicare Advantage plans, Medicaid managed care organizations, Medicaid agencies, TRICARE and the Federal Employee Benefits Plan in addition to Medicare fee-for-service. Taken together, these represent over 50% of all the health care expenditures in the United States and, if they acted in concert to sow the same APM seeds, the transformational impact on the delivery system would be very significant. It may, however, not be enough.
And that’s where private sector, state, municipal and other local government health benefits plans have to step in -- to adopt the same seeds and sow the same crops. Providers need consistency in incentives and concerted action across the public and private sectors would create that consistency.
Organizing around the outcomes we want to achieve
One of the central crops is episode/bundled payment programs covering a variety of conditions and procedures. In the Leavitt Partners report, there are specific recommendations on how episode/bundled payment programs should be structured for maximum effect. For example, how benchmarks are set and prices trended is the difference between success and failure. There are others that anyone serious about implementing episodes of care payment programs should read, understand and apply.
Taken together, these reports lay out a clear pathway for APMs in the next decade or more. Signify Health has fully embarked on this pathway and, with its program sponsors and participants, is showing how the delivery system can be transformed, how outcomes can change for the better when payment changes for the better, and how patients can end up with more, better, healthier days at home and work. We hope you’ll join us.
Topics: Value-based care




